Alzheimer’s Disease is a chronic, progressive, and irreversible neurodegenerative disease that gradually destroys brain cells, leading to a decline in memory, thinking, language, judgment, and eventually independence in daily functioning. It is the leading cause of dementia globally. The most common cause of dementia.
Healthcare providers can suggest treatments to manage symptoms, but there’s no cure for Alzheimer’s disease. Alzheimer’s disease accounts for 60-80% of dementia cases. Alzheimer’s is not a normal part of aging. The greatest known risk factor is increasing age, and the majority of people with Alzheimer’s are 65 and older. Alzheimer’s disease is considered to be younger-onset Alzheimer’s if it affects a person under 65. Younger-onset can also be referred to as early-onset Alzheimer’s. People with younger-onset Alzheimer’s can be in the early, middle or late stage of the disease.
History
- First described by Dr. Alois Alzheimer in 1906.
- Observed a 51-year-old woman with memory loss and psychiatric symptoms.
- Post-mortem showed brain atrophy, amyloid plaques, and neurofibrillary tangles.
Epidemiology of Alzheimer’s disease (Global & India Specific)
- Worldwide: >55 million people living with dementia (WHO 2024), 60–70% are Alzheimer’s.
- India: ~7.6 million people expected to have dementia by 2030.
- Age: Risk doubles every 5 years after 65.
- Sex: Women are disproportionately affected (due to longevity + hormonal factors).
- Urban vs. Rural: Diagnostic gap higher in rural populations.
Alzheimers worsens over time. Alzheimer’s is a progressive disease, where dementia symptoms gradually worsen over a number of years. In its early stages, memory loss is mild, but with late-stage Alzheimer’s, individuals lose the ability to carry on a conversation and respond to their environment. On average, a person with Alzheimer’s lives four to eight years after diagnosis but can live as long as 20 years, depending on other factors.
Etiology of Alzheimer’s disease (Causes and Risk Factors)
A. Genetic Factors
- Early-Onset AD (before 65): Rare (<5%), inherited in autosomal dominant pattern.
- Mutations: APP, PSEN1, PSEN2
- Late-Onset AD: Common; risk associated with APOE-e4 allele (dose-dependent risk).
B. Environmental & Modifiable Factors
- Cardiovascular disease (hypertension, stroke, diabetes, hyperlipidemia)
- Head trauma or concussion
- Sedentary lifestyle
- Smoking and alcohol use
- Chronic stress and sleep apnea
- Depression
- Poor diet and lack of social stimulation
C. Non-Modifiable Factors
- Age
- Gender (female)
- Family history
Early symptoms of Alzheimer’s disease include forgetting recent events or conversations. Over time, Alzheimer’s disease leads to serious memory loss and affects a person’s ability to do everyday tasks.
Pathophysiology (Mechanisms of Damage)
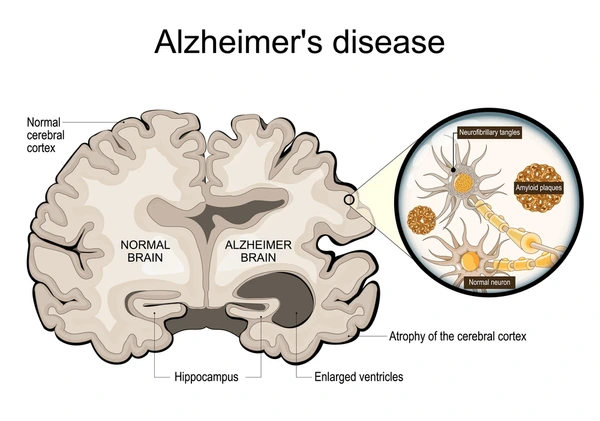
Two abnormal structures called plaques and tangles are prime suspects in damaging and killing nerve cells.
- Plaques are deposits of a protein fragment called beta-amyloid (BAY-tuh AM-uh-loyd) that build up in the spaces between nerve cells.
- Tangles are twisted fibers of another protein called tau (rhymes with “wow”) that build up inside cells.
1. Amyloid Cascade Hypothesis
- Misprocessing of Amyloid Precursor Protein (APP) → β-amyloid → extracellular plaques
- Plaques disrupt neuron communication and trigger inflammation
2. Tau Pathology
- Abnormal phosphorylation of tau protein → neurofibrillary tangles (NFTs) inside neurons
- Blocks microtubule transport → cell death
3. Brain Structural Changes
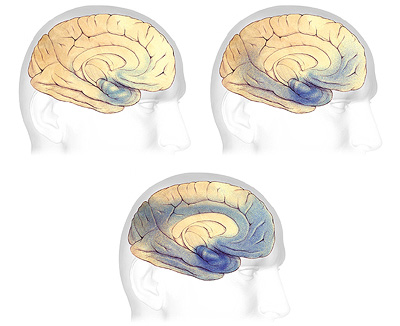
- Shrinkage of hippocampus (early)
- Atrophy of cerebral cortex
- Widened ventricles
- Loss of cholinergic neurons
4. Additional Mechanisms
- Oxidative stress, mitochondrial dysfunction
- Neuroinflammation
- Blood-brain barrier dysfunction
Clinical Features: Signs and Symptoms
Cognitive Impairments
- Short-term memory loss (earliest sign)
- Poor judgment and decision-making
- Disorientation (time/place)
- Language difficulties (aphasia)
- Difficulty with complex tasks
Behavioral and Psychological Symptoms of Dementia (BPSD)
- Depression, anxiety
- Irritability, aggression
- Wandering
- Hallucinations or delusions (later stages)
- Sleep disturbances
Functional Impairment
- Loss of independence
- Difficulty dressing, cooking, hygiene
- Eventual complete dependency
Cleveland clinic article about– Alzheimer’s disease
Stages of Alzheimer’s Disease
| Stage | Features |
|---|---|
| Preclinical | No symptoms, biomarkers abnormal (amyloid, tau) |
| Mild Cognitive Impairment (MCI) | Memory issues but functional independence maintained |
| Mild Alzheimer’s | Noticeable memory loss, word-finding issues, misplacing items |
| Moderate Alzheimer’s | Increased confusion, personality changes, wandering |
| Severe Alzheimer’s | Loss of communication, mobility, bladder/bowel control |
Diagnosis of Alzheimer’s
Clinical Criteria (DSM-5, NIA-AA
Insidious onset and progressive worsening
Memory + ≥1 cognitive domain impairment
Functional decline
Cognitive Assessments
MMSE (Mini Mental State Exam)
MoCA (Montreal Cognitive Assessment)
Clock Drawing Test
Laboratory & Imaging
MRI/CT: Cortical atrophy, hippocampal shrinkage
PET: Amyloid or Tau PET (advanced settings)
CSF: Decreased Aβ42, increased total tau and phosphorylated tau
New blood tests: Detect plasma biomarkers like p-tau217, NfL (under research)
Treatment Approaches
Pharmacological
- Symptomatic Drugs:
- Donepezil, Rivastigmine, Galantamine (cholinesterase inhibitors)
- Memantine (NMDA antagonist)
- New Disease-Modifying Drugs:
- Lecanemab (Leqembi) – FDA approved 2023
- Donanemab – Approved 2024 conditionally
- Work by clearing amyloid plaques but need early diagnosis
Non-Pharmacological
- Memory aids and cognitive training
- Regular physical activity
- Music and art therapy
- Behavioral therapy
- Environmental modifications for safety
Caregiver and Social Support
- Emotional and physical burden is high
- Education and counseling
- Respite care
- Alzheimer’s support groups
- Long-term planning: legal, financial, end-of-life care
Prevention Lifestyle Interventions (The “7 Pillars”)

- Exercise (aerobic + resistance)
- Nutrition (Mediterranean diet)
- Mental stimulation (learning new skills)
- Sleep hygiene
- Social engagement
- Stress reduction (yoga, mindfulness)
- Managing chronic illness (BP, diabetes, cholesterol)
Research & Future Directions
Hot Research Areas
- Amyloid and tau targeting immunotherapies
- Gene therapy and stem cell-based neural regeneration
- AI-powered diagnostic tools
- Blood biomarkers for early, affordable diagnosis
- Brain-gut microbiome connection studies
Major Global Initiatives
- WHO Global Action Plan on Dementia (2017–2025)
- Alzheimer’s Association’s clinical trial database
- India: National Program for Health Care of the Elderly (NPHCE)
MUST READ – Parkinson’s disease: What it is, how to manage and 10 ways to prevent it.
Nutriphyfit
Nutrition | Physiotherapy | Fitness


Pingback: Hepatitis B: What is that, Clinical features and 10 Signs and Symptoms. - Nutriphyfit